Contemporary research supports the idea that chronic pathogen infections can:
• Trigger or worsen autoimmune diseases through misdirected immune responses
• Increase cancer risk both directly and via long-term inflammation
• Engage immune regulatory pathways shared between infection, autoimmunity, and tumor biology
This is a multifactorial interplay rather than a single cause-effect relationship — genetics, environment, and immune history all shape individual outcomes.
Chronic immune activation drives systemic inflammation
Persistent infections keep the immune system in a prolonged “alert” state, producing pro-inflammatory signals (cytokines like IL-6, TNF-α). Chronic systemic inflammation is a recognized risk factor for:
- Autoimmune disorders
- Cancer development and progression
- Cardiovascular, metabolic, and neurodegenerative diseases
This inflammatory milieu damages tissues and alters regulatory immune responses over time, increasing disease susceptibility.
Mechanisms connecting infections and autoimmunity
Multiple biological processes can trigger or exacerbate autoimmune diseases when pathogens persist:
- Molecular mimicry: Pathogen proteins closely resemble human proteins, causing the immune system to attack both.
- Epitope spreading: Immune responses to infection expose additional self-antigens, expanding the autoimmune attack.
- Bystander activation: Inflammation and immune activation indirectly activate autoreactive immune cells.
These mechanisms have been documented for viruses, bacteria, parasites, and fungi.
Examples include:
- EBV and autoimmune diseases such as multiple sclerosis and lupus (epidemiological links and emerging causal data)
- Respiratory and enteric infections associated with autoantibodies or autoimmune sequelae
- Certain bacterial infections that may contribute to autoimmune thyroiditis in predisposed individuals
These findings point to complex immune misdirection rather than simple infection alone.
Chronic infections contribute to cancer risk
Pathogens can influence cancer development through direct and indirect routes:
Direct oncogenic infection
Some pathogens carry oncogenes or transform host cells:
- Human papillomavirus (HPV) → cervical and other cancers
- Hepatitis B and C viruses → liver cancer
- Certain retroviruses and oncoviruses → lymphomas or other malignancies
Overall, infections are estimated to contribute to ~15–20% of human cancers worldwide.
Indirect cancer-promoting effects
Chronic infection → persistent inflammation → DNA damage and proliferation → increased transformation risk:
- Chronic parasitic infections (e.g., Schistosoma hematobium) are linked with bladder cancer
- Helicobacter pylori infection is a strong risk factor for gastric cancer
- Long-standing bacterial and parasitic infections may promote malignant changes via inflammation and cell turnover
These relationships are supported by epidemiological and biological evidence, though the strength of associations varies by pathogen.
Immune system overlap: autoimmunity and cancer
Recent research highlights that:
- Immune dysregulation is central to both autoimmune disease and cancer, with shared immune pathways
- Certain immune cell types (like regulatory T cells) behave differently in cancer versus chronic infection settings
- Autoimmune patients may have altered cancer risk patterns depending on disease type and immune profile
This suggests that chronic infection-induced immune changes can ripple across disease categories.
Examples showing real biological links
- Epstein-Barr virus (EBV) is nearly universal but in some individuals appears to trigger lupus and other autoimmune diseases, with research linking infected immune cells to autoreactivity.
- Chronic bacterial infections like H. pylori are established risk factors for gastric cancer.
- Long-standing parasitic infection (Schistosoma) contributes to bladder cancer via inflammation and cell proliferation.
Key mechanisms scientists are studying
- Inflammation and cytokine dysregulation: Sustained immune signals damage tissues and promote genomic instability.
- Immune tolerance breakdown: Chronic antigen exposure can undermine self-tolerance.
- Oncoviral integration: Viral genomes may integrate into host DNA and disrupt tumor suppressor/oncogene networks.
- Microbiome and metabolic shifts: Chronic infection alters microbial balance and metabolic signals, influencing immunity and cancer risk (emerging area of research).
Summary conclusion
From a biological, immunological, and preventative-health perspective, it makes clear and rational sense to perform regular pathogen cleansing alongside lymphatic and detox pathway support—especially in midlife. Also, by 45 to 60 years old you can have accumulated up to 15kg’s of backed up waste!
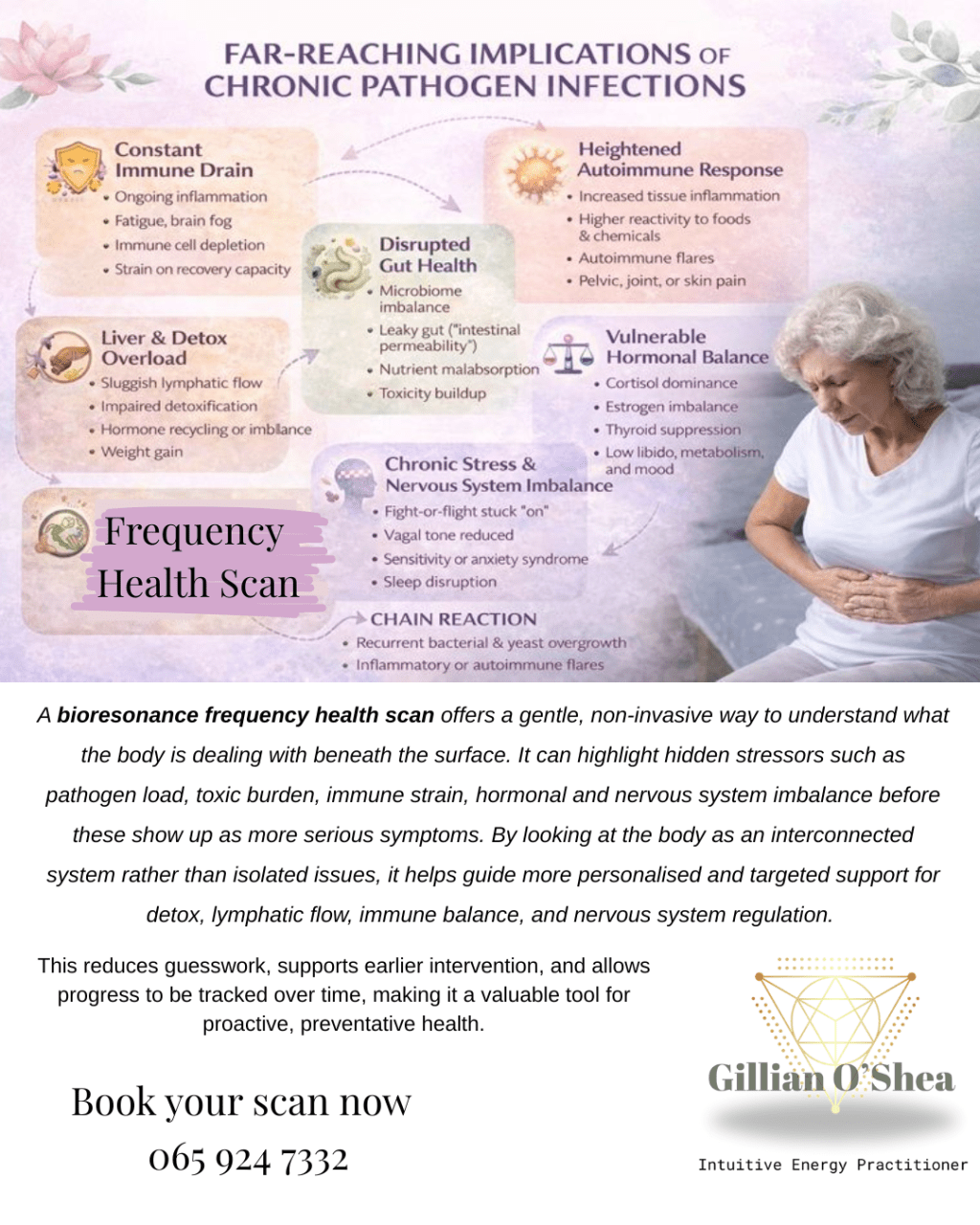
Chronic pathogens persist quietly, placing a continuous low-grade burden on the immune system, driving inflammation, disrupting the microbiome, and interfering with hormonal, neurological, and metabolic balance. Over time, this constant immune engagement increases vulnerability to autoimmune dysregulation, chronic inflammatory conditions, and cancer-promoting environments.
However, pathogens are only part of the picture.
The body’s ability to clear them safely depends on:
- Efficient lymphatic flow
- Functional liver and detox pathways
- A regulated nervous system
- A resilient gut-immune interface
When lymph and detox systems are congested or overwhelmed—due to stress, hormonal shifts, toxic load, or aging—pathogens, inflammatory byproducts, and metabolic waste are more likely to linger, recirculate, and amplify immune confusion. This is when symptoms become chronic rather than self-resolving.
Regular, gentle, well-timed pathogen cleansing, combined with consistent lymphatic and detox support, helps:
- Reduce chronic immune activation
- Lower systemic inflammation
- Prevent toxic and microbial accumulation
- Restore immune precision rather than immune overreaction
- Protect long-term cellular and tissue health
Importantly, this is not about aggressive detoxing or constant “cleansing.” It is about respecting biological rhythms, supporting elimination pathways, and preventing overload before dysfunction sets in.
It’s a proactive maintenance practice, when done intelligently and gently, it supports resilience, immune clarity, and vitality across the lifespan—particularly during the recalibration phase of midlife.




Leave a comment